Steven N Gold, PhD is Professor Emeritus, Nova Southeastern University (NSU) College of Psychology, and was Founding Director of NSU’s Trauma Resolution & Integration Program (TRIP). He has served as President of the American Psychological Association (APA) Division of Trauma Psychology (56), inaugural editor of the Division’s scientific journal, Psychological Trauma from 2008 through 2014, recipient of the Division’s Award for Outstanding Service to the Field of Trauma Psychology in 2014, the Division’s Lifetime Achievement Award in 2022, and was a Div56 delegate to the APA Council of Representatives. In 2004 Dr. Gold served as President of the International Society for the Study of Trauma and Dissociation (ISSTD); he received ISSTD’s 2020 Cornelia B Wilbur Award for outstanding clinical contributions to the treatment of dissociative disorders and ISSTD’s 2022 Lifetime Achievement Award. He is a Fellow of ISSTD and of APA. Dr. Gold has published and presented on abuse, trauma, dissociation, hypnotherapy and psychedelic-assisted therapy, and has been an invited speaker throughout the United States and in Canada, Colombia, Argentina, Spain, Switzerland, and Austria. He is Editor in Chief of the APA Handbook of Trauma Psychology, a Co-Editor of the second edition of the book Dissociation and the Dissociative Disorders, and author of the books Contextual Trauma Therapy for Complex Traumatization and Not Trauma Alone. Dr. Gold was founding co-editor of the Journal of Trauma Practice, and guest edited a special issue of the APA journal Psychotherapy on the treatment of trauma-related disorders. He is a Certified Traumatologist with the Traumatology Institute, a Certified Consultant in Clinical Hypnosis with the American Society of Clinical Hypnosis and sits on the Board of Directors of the Sidran Institute for Traumatic Stress Education and Advocacy and on the Advisory Board of the Leadership Council on Child Abuse & Interpersonal Violence. Dr. Gold maintains an independent psychology practice in Plantation, Florida and is regularly retained as an expert witness in legal cases in which trauma and dissociation appear to be relevant issues.
Jessica Endres, LPC, MA, NCC is a Licensed Professional Counselor in her private practice in Texas called Red Oak Therapy, PLLC. In her practice, she provides individual counseling, virtual DBT group counseling, consultation for working with trauma and dissociative disorders, and training or speaking engagements. She works with adults who have experienced neglect and sexual, physical, or emotional abuse. Most of her clients are working to manage attachment issues, personality disorder symptoms, PTSD, complex PTSD, and dissociative disorders. Jessica has previous clinical experience in various settings including a psychiatric hospital, local mental health authority, rape crisis center, and domestic violence shelter. Her clinical training includes Dialectical Behavioral Therapy and Eye Movement Desensitization and Reprocessing (Basic, PRECI, ASSYT, Group). Additionally, she is a trained yoga instructor and integrates mindfulness and the various limbs of yoga into her practice. Presently she is also a doctoral candidate in Counselor Education and Supervision at Sam Houston State University. In her research, she focuses on the identification and treatment of dissociation and dissociative identity disorder (DID). Personally, she is an extroverted, social person who enjoys playing sports and spending time with her dogs and loved ones.
Lexi M is trauma educator, survivor outreach provider, and co-founder of Beauty After Bruises. As a survivor of highly complex trauma herself, she uses her lived experience of Dissociative Identity Disorder, as well as navigating all levels of treatment, to inform her outreach and advise clinicians, survivors and everyone with BAB. Due to the nature of her trauma story, much of her personal credentials and life identifiers maintain a level of anonymity, which has become a unique opportunity to demonstrate healthy boundaries and show one potential path concerned survivors can take in their passions. Lexi's main focus today is in creating clear, well-synthesized, heartfelt psychoeducation; writing articles, symptom management tools and resource guides; designing social media and web materials; and most of all bridging the gaps between all extremes necessary for trauma care. Matching well-researched data with deep heart and connection, healthy realism with flourishing hope, and compassionate awareness with real tangible and effective change.
Anne Knisley is the Co-founder and Survivor Outreach Liaison for the nonprofit organization Beauty After Bruises. Beauty After Bruises directly helps survivors with Complex PTSD and Dissociative Disorders access the therapeutic and inpatient care they need by providing financial grants as well as bridging the many gaps in trauma care by locating specialized clinicians, educating the public on trauma and dissociation, and giving survivors themselves the tools and self-compassion needed to fight another day
Anne received her BA from York College of Pennsylvania and built her career and businesses ownership in the health and human services industry. After life was redirected by a loved one's close and intimate battle with complex trauma, her focus transitioned into becoming an effective support person in their life. This required a robust crash course in trauma and dissociative disorders, the bureaucracy and financial demands of the healthcare industry, and society's mistreatment of survivors. This early introduction and life milestone birthed a passion to ensure the same services reach the countless survivors that did NOT have anyone in their corner to guide them through this maze. Thus, the Beauty After Bruises initiative was born.
Today Anne mainly works one-on-one with our survivors, their therapists, and doing public education. In every role, she offers the information, skills, and self-confidence needed to proceed with strength, self-agency and the knowledge that someone has their back.
On March 5th, we helped with the first ever DID Awareness Day webinar from ISSTD!
This event was hosted as a panel, with speakers from An Infinite Mind, Beauty After Bruises, and the Blue Knot Foundation.
Thank you for all who joined us!
You can watch the video of the webinar HERE:
Richard P. Kluft, M.D., Ph.D., practices psychiatry, psychoanalysis, and medical hypnosis in Bala Cynwyd, PA. He is Clinical Professor of Psychiatry at Temple University School of Medicine. He serves on the faculty of the Psychoanalytic Center of Philadelphia, where he is a Waiver Training Analyst, and on the faculty of the China American Psychoanalytic Alliance.
He has published over 260 scientific papers and book chapters. Most of these papers concerned trauma, dissociation, dissociative disorders, therapeutic impasses, boundary violations, hypnosis, and psychoanalysis. His recent book, Shelter from the Storm (2013), explorating a compassionate approach to the abreaction of trauma, won the 2013 Written Media Award of the International Society for the Study of Trauma and Dissociation. His edited books are Childhood Antecedents of Multiple Personality, Treating Victims of Sexual Abuse, and Incest-Related Syndromes of Adult Psychopathology. He and Catherine G. Fine, Ph.D., co-edited Clinical Perspectives on Multiple Personality Disorder. Dr. Kluft was Editor-in-Chief of the journal DISSOCIATION for ten years. He is currently Clinical Forum Editor of the International Journal of Clinical & Experimental Hypnosis and Advisory Editor of the American Journal of Clinical Hypnosis. He has presented over 1,000 scientific papers and workshops.
He was a co-founder and an early President of the International Society for the Study of Trauma and Dissociation. He has been President of the American Society of Clinical Hypnosis and the Society for Clinical and Experimental Hypnosis, and International Conference Chair of the International Society of Hypnosis. He has received numerous awards for his published research and his clinical and teaching contributions. These include four Erickson Awards for the best scientific paper of the year in hypnosis, and the 2019 Ernest R. Hilgard Award for the best paper addressing the history of hypnosis. The Journal of Trauma and Dissociation has established the Richard P. Kluft, M.D. Award to honor its best scientific paper of the year. He has held several visiting professorships.
He was the Director of the Dissociative Disorders Program at The Institute of the Pennsylvania Hospital for 8 years. He has extensive experience in treating victims of sexual exploitation by psychotherapists and has served as an expert witness in several malpractice cases involving boundary violations. He also has served as an expert witness in cases in which the diagnosis of dissociative disorders or matters of memory were major issues, including those involving murder and serial murder charges. Dr. Kluft served as a consultant to the Dreamworks and Showtime series, “The United States of Tara.” He was featured in the Showtime documentary, “What Is DID? With Richard P. Kluft, M.D,” which won the 2009 Media Award of the International Society for the Study of Trauma and Dissociation.
He has a second career as a writer of novels and short stories. He is the author of three novels Good Shrink/Bad Shrink (2014), An Obituary to Die For (2016) and A Sinister Subtraction (2019), and a novella, How Fievel Stole the Moon: A Tale for Sweet Children and Sour Scholars (2014).
Elizabeth Power, M. Ed., CEO of EPower & Associates, Inc. epowerandassociates.com, is a sought-after speaker, facilitator, teacher, and consultant. EPower & Associates is the parent organization for The EPower Change Institute and The Trauma Informed Academy.
"All I do is help people with change, resilience and self-care, and alignment. And everything is done from the trauma-informed perspective," she says. "Even courses directly about working with trauma are about change."
Power develops cross-cultural adaptations of models of care for the mental health community as well as helping other countries like Japan develop their own models. The Trauma Informed Academy recently released her new model, The Trauma Responsive System which focuses on mastering 9 elements akin to applied emotional intelligence.
She was recently published as third author of an article in Family Medicine about the outcomes of the NIMH research project assessing the effectiveness of the use of the core principles of Risking Connection(r) by Primary Care Providers in their clinical settings.
When organizations and associations book her as a speaker, it’s most often for motivation, to help people make and adapt to change, or to tell her own story of hope and healing. Conferences love her for her interactive virtual presentations on change, resilience and self-care, and trauma-informed thinking.
“Sharper than a number two pencil, and funnier than a six pack of funny bones on go-juice,” was one audience member’s response. When you need a speaker with humor, depth, wisdom and motivation, she’s the one.
Scroll down for audio/video/print material, or contact us to discuss bookings.
Dr. Mary-Anne Kate is an award-winning post-doctoral researcher specialising in interpersonal trauma, attachment, and post-traumatic disorders.
She is a Scientific Committee member of the International Society for the Study of Trauma and Dissociation, where she also teaches the introductory course on dissociation alongside Christine Forner.
Mary-Anne is the lead author of the chapter on dissociative and somatic disorders in Wiley's Abnormal Psychology textbook, and has written articles on post-traumatic disorders, including dissociative disorders complex PTSD, and borderline personality disorder.
Mary-Anne also has over a decade's experience as a senior policy officer in Canberra, a program manager in Cairo, and a policy analyst in Brussels improving quality of life outcomes, including mental health, for vulnerable client groups such as migrants, refugees, and other minorities.
Mary-Anne lives on the mid-north coast of New South Wales in Australia and currently teaches on the Master in Mental Health program at Southern Cross University, and holds an adjunct research position at the University of New England.
This week we welcome to the podcast nutritionist Annie Goldsmith:
Annie Goldsmith, RD, LDN holds an undergraduate degree from the University of Rochester in Brain and Cognitive Sciences and attended Winthrop University for her graduate coursework in human nutrition.
She has worked in eating disorder treatment at the Partial Hospitalization Program, Intensive Outpatient Program, and outpatient levels of care.
She founded her group practice, Second Breakfast Nutrition, in 2015; her practice is rooted in the Health at Every Size® and Intuitive Eating philosophies.
She has presented on weight-inclusive care at the NCAND regional meeting and at the annual AHEC diabetes symposium in Charlotte, NC.
Annie became interested in somatically-oriented and trauma-informed approaches to nutrition therapy in eating disorder treatment in 2018, when she began training with the Embodied Recovery Institute.
She realized that an understanding of how nervous system state impacts eating is missing from many traditional approaches to ED treatment.
She is passionate about bringing the body into the conversation and providing education to colleagues about trauma-informed approaches to nutrition therapy.
You can see her website HERE and her Instagram is @second_breakfast_nutritionclt
Laura S. Brown, Ph.D. is a clinical and forensic psychologist in independent practice in Seattle, Washington. A speaker and author on feminist therapy theory and practice, she offers workshops and trainings to professionals and the public on such topics as trauma treatment, cultural competence, psychological assessment, and ethics.
Dr. Brown grew up in Cleveland Heights, Ohio where she first became active in movements for social justice that have shaped the direction of her life’s work. Choosing a career in psychology over one as a vocalist, she received a B.A cum laude in 1972 from Case Western Reserve University, and a Ph.D. in Clinical Psychology from Southern Illinois University at Carbondale in 1977. She completed a predoctoral internship in Clinical Psychology at the Seattle Veteran’s Administration Medical Center.
Dr. Brown has served on the faculties of Southern Illinois University, the University of Washington, and the Washington School of Professional Psychology, and has taught and lectured through the U.S., Canada, Europe, Australia, Taiwan and Israel. In the early 1980s she hosted one of the first radio call-in shows by a psychologist.
The bulk of her scholarly work has been in the fields of feminist therapy theory, trauma treatment, lesbian and gay issues, assessment and diagnosis, ethics and standards of care in psychotherapy, and cultural competence. She has authored or edited fourteen professional books including the award-winning Subversive Dialogues: Theory in Feminist Therapy as well as more than 150 other professional publications, and has been featured in six psychotherapy training videos.
A full list of her written work is HERE.
Her written work about Feminist Therapy is HERE.
She is also the author of two books for survivors:
Not the price of admission: Healthy relationships after childhood trauma
Your turn for care: Surviving the aging and death of the adults who harmed you
You can read more about Dr. Laura Brown and her work on her website HERE.
Melissa C. Water is part of “The Bag System” and is working toward creating a desktop application for assisting communication in Dissociative Identity Disorder systems. She has fully designed the concept behind the app’s features and options. The website where you can find the video with the detailed mock-up of the app can be found at multipliedbyone.com.
If you are available to donate time to coding the app, please contact Melissa directly at contact@multipliedbyone.com.
Melissa has been recently diagnosed with DID and has spoken of this on her YouTube channels, “Idranktheseawater” and “Coming Inside Out.” Melissa has been on radio shows, podcasts, spoken at conferences, and has been a guest on Canadian Television documentaries on the topic of Tourette syndrome, for which she advocates. The shows were “Employable Me,” and “You Can’t Ask that,”
Melissa started a movement following the trending #GetSplitOffNetflix hashtag on Twitter where rather than focusing on what we are not, we talk about our raw reality by posting about #HumanizingOurDIDTruth @OurDIDTruth
Mark Linington is an attachment-based psychoanalytic psychotherapist with The Bowlby Centre and the Clinic for Dissociative Studies in London UK.
From 2013-2018 he was Chair of the Executive Committee at The Bowlby Centre, where he continues to work as a training therapist, clinical supervisor and teacher. He worked for 12 years in the NHS as a psychotherapist with children and adults with intellectual disabilities, who experienced complex trauma and abuse. He also worked as a psychotherapist for several years at a secondary school in London for young people with special
needs, including autism, ADHD and other intellectual disabilities. He has written a number of papers and book chapters about his clinical work and presented papers on attachment theory in clinical practice at a number of conferences, including in South Korea, Hong Kong and Paris.
He is Clinical Director and CEO at the Clinic for Dissociative Studies, where he is also a specialist consultant psychotherapist and supervisor working with people with Dissociative Identity Disorder (D.I.D.). He works in private practice working with children, adults and families, providing supervision to individuals and groups and training to organisations.
Our guest this week was Richard Schwartz, PhD, who developed the Internal Family Systems (IFS) model of treatment for trauma and other therapeutic issues:
Richard Schwartz began his career as a systemic family therapist and an academic. Grounded in systems thinking, Dr. Schwartz developed Internal Family Systems (IFS) in response to clients’ descriptions of various parts within themselves. He focused on the relationships among these parts and noticed that there were systemic patterns to the way they were organized across clients. He also found that when the clients’ parts felt safe and were allowed to relax, the clients would experience spontaneously the qualities of confidence, openness, and compassion that Dr. Schwartz came to call the Self. He found that when in that state of Self, clients would know how to heal their parts.
A featured speaker for national professional organizations, Dr. Schwartz has published many books and over fifty articles about IFS. You can read more about him and about IFS on his website HERE.
Our guest this week was Jess from the YouTube channel Multiplicity and Me.
The BBC Documentary they received an award for about Dissociative Identity Disorder can be seen here:
The “360 Project” Jess referenced is here:
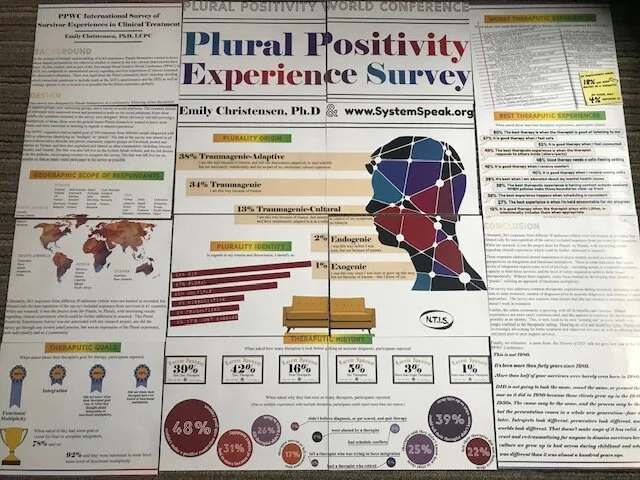
On today’s podcast, we share the PPWC Survey Results about Plural Experience, as an expression of plural culture and shared experiences. These results were accepted for a Poster Session at the 2020 ISSTD Conference in San Francisco. However, as you now know, the conference was cancelled at the last minute due to efforts of government officials’ attempts at controlling the Coronavirus through social distancing. Because we were not able to share our poster, we did take pictures of it and do share them below.
As part of the 2019 Plural Positivity World Conference (PPWC), we helped with a survey with results to be shared in 2020. This Plural Positivity Experience survey was not associated with any research project, nor did the survey go through any review panel process. There was input from the Plural community itself, including deciding which contextual questions to include (such as the ACE’s questionnaire) as well as verbiage options to be as inclusive as possible for the Plural experience. Again, this was not a research project, but was an expression of the Plural experience, both individually and as a community.
Please note:
Participants were informed that the survey results would be shared during the 2020 PPWC Conference.
To continue the survey, participants had to agree that they understood this and that they were over 18.
Any participant who did not agree to have their results shared or who were under 18 were excluded from the survey results published below.
It was explicitly stated, and participants agreed to understanding, that the questions were only for information about their experiences and not at all diagnostic in nature.
Participants were also warned that due to the nature of trauma-specific questions, they could be triggered during the survey. Resources and referrals for support were offered, and system-wide self care was encouraged before, during, and after participating in the survey.
SURVEY DESIGN
This survey was designed by plurals themselves, as a community, following online discussions in support groups, peer mentoring groups, and a variety of social platforms. The common threads of interest were narrowed down and presented in polls on the social platforms. From these results, the questions included in the survey were designed. While obviously vast and covering a multiplicity (pun intended) of areas that would be too many variables for a research project, this was again just the general areas of experience that plurals themselves wanted to know more about and were interested in learning in regards to shared experiences.
The survey was in English.
The survey took an average of 26 minutes to complete.
The first page of the survey was simply exclusionary material clarifying the purpose, concerns, and limitations of the survey. Any “no” responses exited the participant from the survey. Questions included:
I am over the age of 18.
I understand the screening tools used in this survey are for data gathering only, and not meant to be diagnostic in nature.
I understand that due to the nature of the survey in regards to trauma and dissociation, some of the questions may be triggering. I am safe and able to care for myself during and after this survey, and know where and how to seek support if I need help.
I understand I can quit this survey at any time.
I understand the data gathered from this survey is non-identifiable, and that the survey is done with SSL encryption.
I understand that the data results will be combined, and that the overall results will be shared in the Plural Positivity World Conference for plurals, by plurals. I understand that the data results will be shared with the conference via the System Speak podcast, which is a public podcast already on air. I understand that the podcast may be linked to from other blogs, YouTube Channels, and support groups online. I understand that, while this is not an official research project, the clinical community as a whole may have access to these results generally and the related non-identifiable data.
I understand these things and consent to this survey.
The second page of the survey were demographics, including country, identified gender, body age, levels of education for self and each parent. It also included context questions regarding perception of trauma impact on education, frequented online resources, government assistance, housing stability, and patterns of sleeping, eating, and exercise.
The third page of the survey were the questions from the Dissociative Experiences Scale, again clarified that this was for appropriateness of the survey and not for diagnostic purposes.
The fourth page of the survey were the ACE (Adverse Childhood Experiences) questions.
The fifth page of the survey was about therapeutic experiences, including: number of therapists prior to diagnosis, number of therapists since diagnosis, reasons for changing therapists, current reported diagnosis, ritual abuse identification, how therapy is paid for, positive and negative experiences with therapists, what does and does not feel safe in therapy, misdiagnosis experiences, treatment goals, and integration perspectives.
The final page of the survey was cultural, about the personal experiences and identification of or with the integration process and views on functional multiplicity.
There were no research analyses done with the data, beyond the collective-per-question results shared below, or any correlation conclusions drawn from this survey due to this not being an actual research project and other obvious limitations to this survey.
That said, we do believe it to be informational about the common experiences of the Plural community as a whole, and that the survey could be informational upon reflection when considering future clinical studies.
SURVEY PARTICIPATION
The PPWC organizers had an initial goal of 100 responses from different people diagnosed with DID or otherwise identifying as “multiple” or “plural”.
The link to the survey was shared in all known dissociative disorder and plural community support groups on Facebook, posted and shared on Twitter, and then also explained and shared on other communities including Discord, Reddit, and Tumblr.
The link was also left live on this website, and we did discuss it on the podcast.
The link was left live for six months so that as many could participate in the survey as possible.
Ultimately, the survey received 863 responses from different IP addresses (which were not tracked or recorded, but filtered only for non-repetition of the survey).
These responses came from 61 different countries, including:
North America: Canada, United States, Mexico, and Panama;
South America: Columbia, Peru, Brazil, Uruguay, Argentina, Chile;
Europe: Iceland, Ireland, UK, France, Germany, Belgium, Netherlands, Denmark, Norway, Sweden, Finland, Poland, Spain, Portugal, Italy, Slovenia, Austria, Czech Republic, Slovakia, Hungary, Serbia, Romania, Greece;
Africa: Morocco, Ghana, Egypt, Uganda, Kenya, South Africa;
Asia: Turkey, Lebanon, Israel, Iran, Pakistan, India, Nepal, China, Thailand, Cambodia, Indonesia, Philippines, Russia, South Korea, Japan; and
Australia and New Zealand.
The survey had a 92% completion rate. An additional 6% completed more than 75% of the survey, but needed to stop due to length of the survey. 1% had to stop the survey because of triggers. The final 1% did not complete the survey and did not explain why.
RESULTS
PAGE ONE: Clarifying Material and Consent to the Survey
Only participants who answered “Yes” to the first seven questions (see above) were included in the results below.
PAGE TWO: Demographics
Participant countries were listed above.
In regards to identified gender:
54% identified as female;
9% identified as male;
9% identified as non-binary;
8% identified as trans male;
4% identified as gender queer;
3% identified as trans female;
2% identified as gender fluid;
2% identified as non-conforming;
1% identified as gender variant; and
1% identified as questioning.
4% listed “other” as their identified gender, and reported that they did not want to answer.
“Female” and “Trans female” as well as “Male” and “Trans Male” were included separately not to divide the genders (“female” and “trans female” being the same gender, and “male” and “trans male” being the same gender), but simply to clarify experiences in everyone’s request for their journey to be included and reflected.
The remaining percent were decimals in the above percents, as will also be the case with the remaining results below.
In regards to the actual body age, people reported that":
43% were ages 25-34;
20% were 18-24;
16% were 35-44;
13% were 45-54;
2% were 55-64; and
1% was over 65.
We would suggest that the online platforms provided access to younger populations not usually included in research studies. We would also suggest that the online platforms were more accessible to those who are in rural areas and in other geographic locations not usually available to participate in research studies.
In regards to the participants’ fathers’ education:
26% had high school education only;
21% had graduate level education;
20% had bachelor’s level education;
17% had some college but no degree;
7% had an associate’s degree; and
6% did not complete high school.
In regards to the participants’ mothers’ education:
25% had a high school degree only;
18% had some college but no degree;
18% had a bachelor’s degree;
14% had a graduate level education;
11% had an associate’s degree; and
11% did not complete high school.
For participants themselves:
35% have some college education but no degree;
22% have a bachelor degree;
16% have a high school degree only;
11% have a graduate degree;
9% have an associate’s degree; and
4% have not finished high school.
For context, remember that 20% of the participants were in the age group of 18-24; however, that said, more participants have finished high school than their parents. More have some college, even if they have not finished a degree. More have associate’s degrees than their fathers. More have bachelor’s degrees.
Of these, in regards to how their trauma histories impacted their educational efforts, participants reported that:
34% felt their trauma impacted their education “a great deal”;
25% felt their trauma impacted their education “a lot, but I struggled through”;
13% felt their trauma impacted their education “a lot”;
7% felt they were able to complete the education they wanted;
6% felt their trauma “moderately” impacted their education;
5% felt their education was impacted by trauma “some, but I dealt with it okay”;
4% felt their trauma impacted their education “a little”; and
1% felt their trauma did not impact their education.
As for online platforms survivors frequently use for support:
78% use Facebook;
77% use YouTube;
70% use Facebook support groups;
36% use professional and/or clinical research sites;
32% use Twitter;
28% use Podcasts;
24% use Reddit;
22% use Tumblr; and
20% use organizational sites.
As for level of functioning and assistance needed:
59% of participants reported they are not on any social security, housing assistance, or food stamps;
27% of participants reported they are on social benefits;
8% of participants reported they use social benefits, as do others in their household; and
3% of participants reported they do not, but someone else in their household does.
As for housing stability, participants reported that in the last five years:
24% have not moved;
20% have moved once;
15% have moved three times;
13% have moved twice;
7% have moved five times;
7% have moved more than ten times;
4% have moved six times;
2% have moved seven times;
2% have moved four times;
1% have moved eight times; and
1% have moved nine times.
In regards to physical care, the survey included questions about sleep, eating, and exercise.
In regards to sleep, participants reported that:
54% do not exercise at all, due either to preference or medical condition;
21% exercise twice a week;
13% exercise once a week; and
10% exercise five times a week.
No other responses were reported on that question.
In regards to eating, participants reported that:
36% eat twice a day;
24% eat three times a day;
15% eat smaller amounts four times a day;
11% eat just once a day; and
6% reported that eating is difficult, and so they leave food out and “whoever inside” just “grazes” throughout the day if and when they are able to eat something.
In addition,
34% reported they struggle to eat five to six days a week;
20% struggle to eat one to two days a week;
20% do not struggle at all to eat;
18% struggle to eat three to four days a week; and
6% do not miss meals no matter what, nor do they find it difficult to eat.
In regards to sleeping, participants reported that:
28% sleep eight hours or more a night because they have help with medication;
22% sleep six to eight hours a night without the use of medication;
24% sleep four to five hours a night without the use of medication;
21% sleep three to four hours a night without the use of medication; and
4% sleep one to three hours a night without medication.
In addition,
24% rarely have nightmares;
22% have nightmares one to two nights a week;
18% used to have nightmares, but not so much since starting therapy;
15% feel like they still have nightmares every night;
11% have nightmares three to four nights a week; and
7% have nightmares five to six nights a week.
PAGE THREE: Dissociative Experiences Scale (DES) -II
The DES was included for context of what issues participants struggle with and which populations were completing the survey. It was not used for any diagnostic purposes, nor were the results saved in anyway by specific participants. Rather, the algorithm of responses scored this page per participant but only reported in the results of the page in the percentage of participants who scored in each range. So, we were not informed of which DES score goes with which participant. We only know what percentage of each possible DES score. That was intentional, as an additional buffer for privacy since this is not a clinical research study or diagnosis in any way. Participants were not informed of their individual score, nor was this reported to us in anyway. Individual DES-II scores were not reported or disclosed to anyone in any way.
Of the participants in this survey, 89% scored above 30 on the DES-II. 6% scored between 27-30. 4% scored between 24-26. 1% of participants scored 23 or below.
The high scores were expected, due to the population receiving notice of and participating in this survey were primarily those already in treatment for or aware of their own issues of trauma and dissociation.
Please note that higher scores (30 and above) only indicate high levels of dissociation, and are not indicative of specific diagnosis in and of themselves.
Again, the inclusion of the DES-II was only as a measurement of experience in the context of this survey; no clinical interview, structured or otherwise, was part of this survey, and no diagnoses were given to any participant.
For more information about the DES-II, please visit the ISSTD website. To take an online version of the DES-II, CLICK HERE.
PAGE FOUR: Adverse Childhood Experiences (ACE)
We included the ACE questions by request of the community due to increasing discussion within the community of the physiological impact of trauma long-term.
The ACE study questions were broken down into the questions listed below, to which participants could answer “yes” or “no”. Again, a specific participant’s answers were not saved per participant, but rather as a poll for how many participants answered yes to each question. This was both in protection of people’s privacy and because the survey was not being given in a clinical setting. 4% of participants opted out of this page due to the nature of the triggering questions regarding their own trauma. Another 1% declined to participate for other unspecified reasons. The positive results endorsed by those participants who completed this set of questions are given as follows:
Did a parent or other adult in the household often or very often… Swear at you, insult you, put you down, or humiliate you?
80% YES
Did a parent or other adult in the household often or very often… Act in a way that made you afraid that you might be physically hurt?
78% YES
Did an adult or person at least 5 years older than you ever… Touch or fondle you or have you touch their body in a sexual way?
66% YES
Did an adult or person at least 5 years older than you ever… Attempt or actually have oral, anal, or vaginal intercourse with you?
52% YES
Did you often or very often feel that… No one in your family loved you or thought you were important or special?
71% YES
Did you often or very often feel that… Your family didn’t look out for each other, feel close to each other, or support each other?
70% YES
Did you often or very often feel that… You didn’t have enough to eat, had to wear dirty clothes, and had no one to protect you?
44% YES
Did you often or very often feel that… Your parents were too drunk or high to take care of you or take you to the doctor if you needed it? Or didn't for some other reasons?
36% YES
Did a parent or other adult in the household often or very often… Push, grab, slap, or throw something at you?
53% YES
Did a parent or other adult in the household often or very often… Ever hit you so hard that you had marks or were injured?
45% YES
Was your mother or stepmother: Often or very often pushed, grabbed, slapped, or had something thrown at her?
23% YES
Was your mother or stepmother: Sometimes, often, or very often kicked, bitten, hit with a fist, or hit with something hard?
15% YES
Was your mother or stepmother: Sometimes, often, or very often threatened with a gun or knife or other weapon?
4% YES
Were your parents separated or divorced?
49% YES
Did you live with anyone who was a problem drinker or alcoholic or who used street drugs?
47% YES
Was a household member depressed or mentally ill, or did a household member attempt suicide?
72% YES
Did a household member go to prison?
15% YES
It is interesting to note that 7% of participants wished the ACE questions included similar specific questions for their father or stepfather the way it does about the mother or stepmother, as this group of people reported their mothers as the or one of the primary abusers even against their father or stepfather.
PAGE FIVE: Therapeutic Experiences
This section of the survey addressed issues regarding therapeutic experiences that the Plural Community had brought up in discussion about what to include in the survey.
In asking about who was in therapy, the participants responded as follows:
58% were currently in therapy at the time;
10% were, but had to quit because their therapist didn’t “believe” in dissociation;
10% wanted to be, but have been unable to find a therapist who works with dissociation;
8% were, but had to stop when their funding was cut or insurance stopped paying for it;
4% were, but their therapist moved;
4% were not currently, but actively looking for a therapist;
3% were, but had to stop because of schedule conflicts; and
1% were not because they chose not to be in therapy.
Not one person responded that they were in therapy and it was entirely covered by insurance.
When asked about how many therapists they had thus far, participants responded that:
21% had been referred more than six times;
18% had been referred more than seven times;
18% had been referred more than twice;
16% had been referred more than three times;
11% had more than eight therapists already;
10% had more than 10 therapists already; and
only 4% have only been with one therapist.
The remainder of participants have not yet found a therapist.
When asked why they had seen so many therapists, participants responded as follows (due to multiple experiences with different therapists, participants could report more than one reason, so these percentages do not add up to 100):
48% couldn’t make a positive connection with good rapport;
39% could tell their therapist didn’t know what to do with them;
31% had to move because of related instability;
26% felt their therapist didn’t listen to them;
25% had a therapist tell them they didn’t know how to treat them;
22% felt their therapist did not believe them;
17% had a therapist who moved or left an insurance panel;
9% were abused by a therapist;
8% had a therapist who retired;
8% had schedule conflicts;
7% didn’t believe their therapist when they did get diagnosed, or got scared, and so quit therapy; and
6% left a therapist who was trying to force integration.
“Other” comments included experiences of aging out of a particular school or program, therapist not being able to handle gender identity or sexual orientation issues, being too anxious to keep appointments, finances, and being forced to report abusers.
When asked how many therapists it took before getting an accurate diagnosis, the participants responded that:
42% had seen two therapists;
39% still had gotten a proper diagnosis with just one therapist;
16% had to see four therapists;
5% saw six therapists;
3% saw more than eight therapists; and
1% saw more than fifteen therapists prior to getting an accurate diagnosis.
When asked to share their diagnosis if they felt safe doing so, the participant percentages were:
53% DID
15% were not sure;
12% waiting on results of testing or for diagnostic appointments;
8% Complex PTSD
5% PTSD
4% DDNOS
3% OSDD
When asked who did the diagnosing, participants replied that:
54% were diagnosed by a therapist;
24% were diagnosed by a psychiatrist;
23% were diagnosed by case manager or social worker;
5% were diagnosed by a doctor; and
4% were “peer-diagnosed” by a friend who referred them to a clinical professional.
When asked how they identified any experience of S/RA, participants shared that:
56% did not know what the terms were and so did not think it applied to them;
23% knew what the terms were, but also knew it did not apply to them;
7% preferred the term RA/MC (Ritual Abuse/Mind Control);
5% preferred the term (S)RA (Satanic/Ritual Abuse);
4% preferred just the general term of trafficking;
3% preferred the term RA (Ritual Abuse); and
1% preferred the term SRA/MC (Satanic Ritual Abuse / Mind Control).
It is interesting to note that not any single participant chose the more general term of “organizational abuse”, and no single participant endorsed “MC - mind control only”.
When asked about other non-trauma diagnoses:
77% also have Anxiety;
67% also have Depression;
67% have both a Dissociative Disorder and PTSD;
25% have a Panic Disorder;
19% also have OCD;
13% have also been diagnosed with Borderline Personality Disorder;
11% have also been diagnosed with a Bipolar disorder;
6% have another mood disorder diagnosis; and
3% have another personality disorder diagnosis.
When asked about their best therapeutic experiences, participants shared (they could endorse more than one):
80% said the best therapy was when the therapist was good at listening to them;
57% said it was good therapy when they felt safe;
56% said they knew it was good therapy when they got good advice;
52% said it is good therapy when they feel connected;
49% said the best therapeutic experience is when the therapist responds to others inside (alters/parts);
48% said good therapy needs a safe-feeling setting;
45% said it is good therapy when they receive comfort;
40% said it is good therapy when they gain coping skills;
38% said it’s best when they are educated about their mental health issues;
38% said the best therapeutic experience is having access to contact outside sessions WHEN policies make those boundaries clear up front;
38% said the best experience happens when the scheduling is consistent;
27% said the best experience is when they are held accountable for their progress;
27% said the best experience is being able to relax and practice relaxation strategies;
18% said it is good therapy when they get safe hugs (with permission);
13% said it is only a good therapy experience when the office staff also feel safe, both on the phone and for check-in/check-out; and
12% said it is good therapy when the therapist plays with Littles or intentionally includes them when appropriate.
When asked about the most helpful techniques their therapists use, participants responded:
87% Listening
72% Reassurance
64% Playing Together
62% Art Therapy
26% Guided Imagery
26% Psychoeducation
24% EMDR
21% Music
19% DBT
18% Meditation
16% CBT
13% Sensory Therapy
11% Sandtray Therapy
10% Horse or Pet Therapy
8% Progressive Muscle Relaxation
5% Yoga
3% Hypnotherapy
Please note that the above list is not an efficacy rating of which techniques are the most effective or produce the best results. These were simply the comfortable techniques experienced by the participant population of this survey. It does not mean any one of those is better or more helpful than another, and may reflect more frequency of use or access than quality of treatment.
When asked what made them feel NOT safe in therapy, the participants endorsed the following:
65% Not knowing how to help me;
56% Not listening to me;
39% Therapist saying my stories were too hard / too much / too intense for them;
37% Therapists refusing to talk to others inside (alters/parts);
32% Discounting my stories;
30% Therapist talking too much about their own stuff during sessions;
25% Not feeling safe with office staff or in office setting;
21% Not available outside of session;
21% Not knowing about vacations or time off ahead of time for scheduling;
20% Concerns about confidentiality;
19% Boundary violations;
18% Therapist being afraid of my insiders (parts/alters);
16% Sudden movements;
15% Rejection of Littles;
13% Touch without permission, even if it was otherwise safe/appropriate;
13% Lack of eye contact;
12% Texting or taking calls from other people during sessions;
8% Not closing the office door during sessions;
3% Deliberate triggering to prove a point, access a particular alter, or test progress;
2% Inappropriate/unwanted religious discussion; and
2% Falling asleep during sessions.
Of participants asked, 18% had been abused by a therapist.
Of these, only 4% reported it.
Of those in therapy, 82% agree with their therapist on their treatment goals. Some of these goals include:
75% Decrease in Anxiety / Panic;
72% Improved Functioning;
67% Memory Work / Specific Trauma Processing;
67% Improved Internal Communication;
66% Compassion for My Self/ves;
62% Improved Mood;
58% Improved Cooperation;
41% Decrease Lost Time;
40% Maintain Functioning;
34% Remembering;
22% Stabilization and Reduce Self-Harm Behaviors;
15% Reduce Interpersonal Drama with Outside Relationships; and
14% Accepting the Diagnosis.
When asked their therapist’s goal for therapy, participants reported:
50% Functional Multiplicity
5% Integration
Another 20% did not know what their therapist goal was or what they thought about integration or functional multiplicity.
12% did not think their therapist has ever heard of functional multiplicity.
When asked about their own goal for therapy, participants reported:
78% Functional Multiplicity
3% Integration
11% had not yet heard the term “functional multiplicity”
When asked directly if participants ultimately had some goal or vision for final or complete integration, 78% said no.
92% said they were interested in some level of functional multiplicity.
PAGE SIX: Plural Perspectives
The final questions regarding plural perspectives became more specific in regards to identifying with or despite trauma, levels of dissociation, and functional multiplicity or ultimate integration. These questions arose from the efforts at uniting the Plural community as a resource for itself, for Plurals by Plurals, while also respecting individual experiences and understanding the perspectives of the clinical community. The options for responses to these questions came from the Plural community themselves, in exploring options of self-expression as a community culture and not just a clinical diagnosis:
The questions will be listed, with the participant percentage responses following.
In regards to my trauma and dissociation, I identify as:
35% DID
27% Plural
22% Multiple
5% Dissociative
3% Traumatized
2% It’s just baggage
In regards to my trauma and dissociation, I am:
30% In the closet publicly, but have found support groups online;
19% I have told friends, but not my family;
12% Everyone knows, and I consider myself an advocate in some way;
10% I have told my friends and family, but carefully with good boundaries;
4% Everyone knows, but I am not safe enough to advocate culturally;
3% Still in the closet, but at least I “get it” and am trying to deal; and
2% So far in the closet that I still am not sure what’s going on yet.
In regards to my trauma and dissociation, coming out to myself:
64% was a huge relief because everything finally made sense;
42% brutally hard, but at least I knew what was going on;
32% was positive because I found others like me;
18% was so hard / terrifying / confusing that I still can’t even think about it yet;
14% was a good thing because I finally got help; and
7% was not a big deal.
In regards to my trauma and dissociation, coming out to others was:
37% mostly with others online who know what it’s like to be me;
29% not as big a deal as I thought it would be;
27% disappointing because I lost family or friend contacts because of it;
25% okay, and my friends were totally supportive;
24% easier with my friends than my family;
16% terrible because of the repercussions that followed;
14% dangerous, and caused me safety problems; and
13% terrifying, and totally backfired.
I believe my dissociation is:
38% Traumagenic-Adaptive (I am this way because of trauma, and still use dissociation adaptively to deal with life but not necessarily intentionally and not as part of my intentional cultural expression.)
34% Traumagenic (I am this way because of trauma.)
13% Traumagenic-Cultural (I am this way because of trauma, feel mostly in control of my symptoms, and have intentionally adapted to it as a cultural lifestyle.)
2% Endogenic (I was this way before I was born, but not because of trauma.)
1% Exogenic (I was this way since I was born or grew up this way, but not because of trauma - that I know of yet.)
There were NO people who marked the following:
0% Iatrogenic (I am this way because my therapist made me this way.)
0% Iatrogenic-SocioCognitive (I am this way because I internalized and/or copied symptoms seen in friends or online, intentionally or unintentionally.)
0% Iatrogenic-Cultural (I am this way because I internalized symptoms of others intentionally or unintentionally, but did intentionally learn/apply it as a lifestyle.)
Other responses included:
Quoigenic - mixed origin
Endogenic, but heavily and negatively impacted by trauma.
Traumagenic-Neonatal. We developed this way before we were born because our maternal unit was being abused/traumatized while we were in the womb. We were "born ready" for plurality & problems/trauma.
Traumagenic-SocioCognitive
When I was young, I tended to identify with:
65% Books
31% Teachers
31% Movies
24% Video Games
23% Science Fiction Anything
21% Comics
20% Role Playing Games
17% Caregivers
17% Role Models
This final question was included because “fictives” are being commonly dismissed from participating in treatment, and we wanted to explain how technology has impacted the use of introjects in plural systems. Here is a quote from the History of DID talk we gave last year at the 2019 PPWC Conference:
This is not 1980.
It’s been more than forty years since 1980.
More than half of your survivors were barely even born in 1980.
DID is not going to look the same, sound the same, or present the same now as it did in 1980 because those clients grew up in the 1940’s and 1950’s and 1960’s. The cause may be the same, and the process may be the same, but the presentation comes in a whole new generation - four decades later. Introjects look different, persecutors look different, and inner worlds look different. That doesn’t make any of it less valid, and it is cruel and re-traumatizing for anyone to dismiss survivors because the culture we grew up in and had access to during childhood and adolescence was different than it was almost a hundred years ago.
Respectfully Submitted, thank you.
Many thanks to our previous guest, Ellen Lacter, PhD, who shares these spouse resources with us now:
Heather Tuba: Trauma-Informed Support for Partners of Survivors:
https://www.heathertuba.com/articles/
Robin Brickel, LMFT: How to Repair Love with Trauma-Informed Couples Therapy:
https://brickelandassociates.com/trauma-informed-couples-therapy/
How People Heal From Trauma, Thanks to Helpers:
https://brickelandassociates.com/how-to-heal-after-trauma-helpers/
The Significant Other's Guild to Dissociative Identity Disorder:
http://www.toddlertime.com/dx/did/did-guild.htm
The road less travelled: how to support your dissociative partner, Parts One and Two, by Rob Spring:
https://information.pods-online.org.uk/the-road-less-travelled-part-one-how-to-support-your-dissociative-partner/
https://information.pods-online.org.uk/the-road-less-travelled-part-two-how-to-support-your-dissociative-partner/
The risk of rescuing: pitfalls and promises in supporting dissociative survivors (PODS):
https://information.pods-online.org.uk/the-risk-of-rescuing-pitfalls-and-promises-in-supporting-dissociative-survivors/
My unique vantage point – parenting dissociative identity disorder with dissociative identity disorder, by Carol B:
https://information.pods-online.org.uk/my-unique-vantage-point-parenting-dissociative-identity-disorder-with-dissociative-identity-disorder/
10 Tips For Spouses and Partners of Survivors with Dissociative Identity Disorder, by Kathy Broady, MSW
https://www.discussingdissociation.com/2016/06/10-tips-for-spouses-and-partners-of-someone-with-dissociative-identity-disorder/
Sidran: For Survivors and Loved Ones:
https://www.sidran.org/for-survivors-and-loved-ones/
For parenting dissociative children: Diagnosis and Treatment of Youth with Dissociation, by Fran S. Waters (2016)
Partners With PTSD by Frank Ochberg, M.D.:
http://www.giftfromwithin.org/html/partners.html
Loving a Trauma Survivor: Understanding Childhood Trauma’s Impact On Relationships, Robin Brickel, MA. LMFT
https://brickelandassociates.com/trauma-survivor-relationships/
Supporting a Loved One Through PTSD or Panic Attacks:
http://sometimesmagical.wordpress.com/2013/10/26/supporting-a-loved-one-through-ptsd-or-panic-attacks/
How Childhood Sexual Abuse Affects Interpersonal Relationships:
http://ritualabuse.us/research/sexual-abuse/how-childhood-sexual-abuse-affects-interpersonal-relationships/
Supporting Someone Who Has Been Raped or Sexually Assaulted:
http://www.healthyplace.com/abuse/articles/supporting-someone-who-has-been-raped-or-sexually-assaulted/
Patience Press (for Help for trauma survivors, war veterans, family members, friends and therapists):
http://www.patiencepress.com/patience_press/Welcome.html
Preventing Compassion Fatigue: What Veteran Spouse/Partner Caregivers Need to Know:
http://giftfromwithin.org/html/Compassion-Fatigue-What-Veteran-Caregivers-Need-to-Know.html
Training for lay counselors: http://www.helpers.homestead.com
http://www.ksacc.ca/docs/when_your_partner_was_sexually_abused_as_a_child.pdf?LanguageID=EN-US
The Post Traumatic Stress Disorder Relationship: How to Support Your Partner and Keep Your Relationship Healthy, by Diane England (2007)
If The Man You Love Was Abused: A Couple's Guide to Healing by, Marie H. Browne (2007)
Healing Together: A Couple's Guide to Coping with Trauma and Post-Traumatic Stress by Suzanne B. Phillips (2009)
Ghosts in the Bedroom: A Guide for Partners of Incest Survivors, Ken Graber (1991)
Trust After Trauma: A Guide to Relationships for Survivors and Those Who Love Them, Aphrodite Matsakis (1998)
Allies in Healing: When the person you love was sexually abused as a child, by Laura Davis (1992)
All the Colors of Me: My first book about Dissociation, by Ana Gomez, illustrated by Sandra Paulsen (for kids)
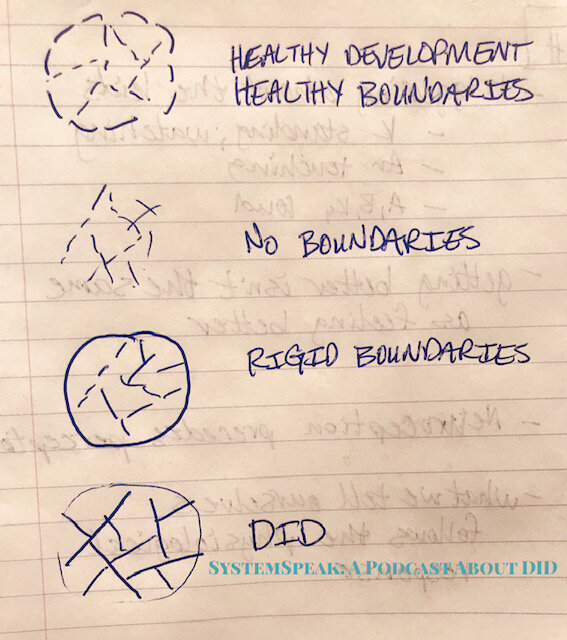
In the episode about Integration and Differentiation, the article that Dr. E found and was sharing is this one:, along with the “pie charts” she referenced during the podcast:
The drawings that our very first therapist did ages ago were something like this, in explaining internal and external walls, and what is helpful and healthy and what makes things more challenging once a survivor is out of danger:
Pam Stavropoulos, PhD
We welcome Pam Stavropoulos, PhD (Politics), Grad. Dip. Psychotherapy to the podcast to share about her research work with complex trauma at Blue Knot Foundation.
Specifically, she shares with us about the recently released 2019 updated Practice Guidelines for the Treatment of Complex Trauma, which you can read HERE. It is available for download for free, with permission to share.
In the podcast, she shares about the research behind the updated guidelines, and also mentions therapist compentancies, which you can read HERE.
A list of selected publications can be viewed HERE.
Dr. Chefetz is a psychiatrist in private practice in Washington, D.C.
He was President of the International Society for the Study of Trauma and Dissociation (ISSTD) from 2002-2003, and is a Distinguished Visiting Lecturer at the William Alanson White Institute of Psychiatry, Psychoanalysis, and Psychology. He is a faculty member at the Washington School of Psychiatry, the Institute of Contemporary Psychotherapy & Psychoanalysis, and the Washington Baltimore Center for Psychoanalysis. . He is a Certified Consultant at the American Society of Clinical Hypnosis and is trained in Level I and II EMDR.
Dr. Chefetz was editor of “Dissociative Disorders: An Expanding Window into the Psychobiology of Mind” for the Psychiatric Clinics of North America, March 2006, “Neuroscientific and Therapeutic Advances in Dissociative Disorders,” Psychiatric Annals, August 2005, and “Multimodal Treatment of Complex Dissociative Disorders,” Psychoanalytic Inquiry, 20:2, 2000, as well as numerous journal articles on psychodynamic and psychoanalytic perspectives on trauma and dissociation. In 2015 he published Intensive Psychotherapy for Persistent Dissociative Process: The Fear of Feeling Real, with W.W. Norton, in their Interpersonal Neurobiology series.
His website is HERE.
This week on the podcast, we discussed an article published by Sarah Clark of the Stronghold System on their website, PowerToThePlurals.com, and shared in her facebook support group AlterNation.
Their article discusses the Theory of Structural Dissociation.
In the article, they consider it to almost be a theory of structural integration instead, and call the theory out for being ableist due to it emphasis on functioning through one ANP in therapy rather than whoever presents, and because of the emphasis on integration as the only treatment option. As they said in the podcast interview, the theory of structural dissociation is being used to push integration as the only option “because it sets up the idea we were never “split off” in the first place, so it’s easier to integrate us back to together again”. Here’s the quote from their article that they reference in the podcast:
We read in the same book (page 7) ‘’Structural dissociation involves hindrance or breakdown of a natural progression toward integration of psychobiological systems of the personality that have been described as discrete behavioral states.’’ (Putnam, 1997).
This is what most people refer to when explaining that we are not broken, not split off. We are all born with different states and early childhood trauma survivors can’t integrate in early childhood due to that trauma. But as you can see it was actually Putnam in 1997 who introduced this idea.
They also say that the authors of the theory appropriated or borrowed terms from other authors who used them much earlier. Here’s a quote from their article:
Charles Samual Myers, who in 1916 wrote about Apparently Normal Part (ANP) and Emotional Part (EP) after acute trauma in WW1. So it is fair to say that the theory of Structural dissociation borrowed these terms, not introduced them, as is readable in the haunted self. (page 4)
Drawing conclusions from this, they clarify that you can accept parts of the theory from the original authors, rather than crediting this theory for your understanding.
They go on to say that the Theory of Structural Dissociation is a model about trauma, not a model about dissociation. Here’s the quote from the article:
It is also good to realize that the theory of Structural dissociation is neither about DID, nor is it about alters, as many of us Plurals know them. They speak of ‘dissociative parts of the personality’, caused by trauma. Nota bene, not early childhood trauma, trauma in general. As this theory also explains single trauma, repeated trauma in adulthood and (early) childhood trauma. It is used to describe changes that are diagnosed as (c)PTSD, trauma related borderline personality disorder, DID and more.
This, along with their perspective that because of DSM5 criteria, DID does not actually have to be a “disorder” if the person’s System is not distressed by it and functioning well. From this, they issue a call to the community to refer to themselves as “Plural” culturally, rather than DID therapeutically. They also are calling for “Functional Multiplicty” to be an option in treatment, rather than integration pushed as the goal.
This, they say, is more effective for positive cooperation amongst a system and healthy functioning as a system, with greater participation in therapy than what the Theory of Structural Dissociation offers. They say:
The theory of Structural dissociation idolizes integration. And although they say that ‘’no one has to go away’’, they also clearly explain to therapists, to not engage with us ‘dissociative parts of the personality,’ unless absolutely needed. Instead it is suggested that the therapist speaks whenever possible, through the ANP fronting…
… And in DID, in particular, requiring all communications to relay through one particular (perhaps malleable or favored) ‘alter’ that sounds a lot like silencing to me. Because the therapist (or any other outside person,) can never know (for sure) whether the part who is presenting, is truly conveying all information which is coming from inside. This book talks a lot about shame, but forgets that our ANPs might not feel comfortable repeating what those EPs just said inside, and that the information may be so overwhelming for them as to cause them to have intense dissociative symptoms.
You can see in the article that they use a picture of a slide from a presentation by Kathy Steele to show that the Theory of Structural Dissociation is being taught to only talk to one ANP and focus on integration in that way.
Following this perspective and logic, they conclude in their article, that the Theory of Structural Dissociation is ableist:
We know from a 6 year follow up study that only 12.8% of participants were able to reach integration as described in the theory of Structural dissociation. (page 4 )
That is a very low percentage. In any scientific research for medicine or therapy for example, a 12.8% positive outcome would not be tolerable. Yet the whole theory of treatment within Structural dissociation is based on it.
A chronic disorder, often debilitating, with a much-respected and idolized healing option with only 12.8% success rate, sounds ableist to me.
A 12% success rate is definitely a call for improved access to and quality in treatment, absolutely, and worth talking about - that’s why we shared it on the podcast.
That said, I don’t know how someone would pin-point integration on a timeline, when to us it feels more like a process than an event (Dr. Siegel said this on our podcast!) - so that 12% seems interesting to qualify with things like how they defined integration and what kind of follow-up support they received and who continued maintenance therapy or not and what kind of life stressors they had and those kinds of questions.
However, there is more to this piece we need to look at to see everything. This study mentioned is one of Bethany Brand’s from Top DD Studies, and I interviewed her earlier for the podcast last summer - unfortunately, it was one of the lost episodes because of technology glitches. But what I know from this study is that it does give a 12% success rate for integration, but it also mentions ANOTHER 12% who are “successful” without integration in a final-fusion kind of way. Further, the study also emphasizes other ways success can be measured and were noticed in the study, including: reduced hospitalizations, reduced suicide attempts, and improved GAF (global assessment of functioning) scores. These are significant and worth mentioning.
But, following this discussion on the podcast, Dr. Peter Barach reached out to us (as a friend and colleague, not in any clinical role) in response with more information. He also clarified that:
I think she has some incorrect ideas about what is generally recommended these days as treatment for DID. I think if you take a look at the ISSTD treatment guidelines, you won’t find what she says to be there. The term “integration” refers to “better integrated functioning ,” not to “fusion” of all the alters I to one.
Kluft argues that fusion leads to the most stable outcome of treatment—that’s his opinion, but the only data on that point comes from a series of people he treated himself. Fusion doesn’t always happen, and it’s also clear that some people with DID don’t want it.
He also shared further insights that we shared in the episode “Clinical Response” in the episode following the interview with the Stronghold System. Here is some of what he clarified in response:
Charles Myers wrote a book (1940) describing veterans of World War I in France who had shell shock, which of course is now called PTSD. He said that there are "emotional" personalities, referring to behavior during flashbacks and trauma-related nightmares, and "apparently normal" personalities who are detached from the experiences of reliving trauma.
I think he used the term "personality" in a much looser sense than we think of parts or alters, whatever word we use, in DID. He was not talking about survivors of childhood trauma.
Myers was not talking about parts or alters with different names and ages. An example of this is a veteran with PTSD working as an auto mechanic who hits the ground when there is a loud noise at work, such as a tire popping suddenly off its rim. This is an automatic response without thinking or planning, and leaves the veteran feeling embarrassed.
Here Dr. Barach clarifies that Myers was not talking about DID, but about a PTSD kind of response. In a plural system, the ANP and EP are distinct personalities as in parts or alters, as in distinguished by identity (age, gender, name, etc.), whereas what Myers was referring to was functioning - the veteran being able to function in a work setting upon returning from war (ANP), but having a limbic response triggered (EP). When Van der Hart uses the terms ANP and EP, he is applying them in an extended way to explain the continuum of dissociation.
Further, Dr. Barach points out that Van der Hart does give Myers credit when using the ANP and EP terminology, so it is neither appropriated or used without acknowledging the source.
Van der Hart always mentions Myers when he uses those terms ANP and EP, so I disagree that he and his coauthors have appropriated or stolen these labels. Van der Hart is also clear that the structural theory of dissociation is talking about ANPs and EPs that are more elaborated than the ANP and EP ideas of Myers.
He then explains this here, using quotes from both Myers and Van der Hart:
Here's what Myers wrote:
"“Now and again there occur alterations of the 'emotional' and the 'apparently normal' personalities, the return of the former often heralded by severe headache, dizziness or by a hysterical convulsion. On its return, the 'apparently normal' personality may recall, as in a dream, the distressing experiences revived during the temporary intrusion of the 'emotional' personality.”
Here's an excerpt from a 2010 article by van der Hart and others:"the EP range in forms from reexperiencing unintegrated (aspects of) trauma in cases of acute and posttraumatic stress disorder (PTSD), to traumatized dissociative parts of the personality in dissociative identity disorder (DID; APA, 1994)."
Dr. Barach then concludes that it’s not accurate to say that Myers was talking about the same thing as DID when he wrote about ANP’s and EP’s, even though that was the original source of the terminology.
He also explained that he wouldn’t consider the OSDD diagnosis as something being used to “step-down” a DID diagnosis, but rather it being related to how the system itself is presenting within the context of what they are dealing with at any given time. He said:
The DSM is a bunch of cubbyholes with labels on them, but the disorders aren't "real" in the same way that a flower or ice cream is real. The DSM is a system of categories. That's all it is.
How things end up in one category or another is a matter of psychiatric politics. For example, PTSD used to be classified as an anxiety disorder. But now it's in the trauma disorder category.
… Well over 95% of people with DID report a history of extensive childhood trauma; there are even some studies confirming the trauma histories of groups of people with DID. But DID is not in the trauma disorders category. It's in the dissociative disorders category. Go figure.
Also the whole issue of OSDD versus DID to me exists only because some psychiatric folks wanted two categories! There are people diagnosed with OSDD whose inner parts never "front," and who don't lose time, unless there is heavy stress. So if I evaluate them on a low stress day, the diagnosis might be OSDD, but an evaluation on a higher stress period of life might lead to a diagnosis of DID.
In regards to whether someone can have DID but it not be a “disorder”, Dr. Barach clarifies that:
“every diagnosis in the DSM requires either "clinically significant distress" or "functional impairment."
So, if one were going for “functional multiplicity”, then that functioning needs to include being able to work, manage relationships, and other ways of functioning. He said:
If someone had parts, wasn't distressed by having them, but wasn't functioning well in relationships or work because of the parts fighting for control or switching a lot, that would count as a disorder.
This put into words what we were trying to explain in the podcast in the follow-up episode, about how (for us) functional multiplicity becomes a natural part of the healing process as internal cooperation and collaboration improves.
In that way, for us, functional multiplicity is a part of the process rather than an end goal alternative to the end of treatment. We - only speaking for our system - are not far enough in treatment to know, experience, or be able to speak of anything else or what we will choose at the end of treatment or understand what that will look like.
However, we understand from our own experience of searching for a good therapist for over a decade, that there is a critical time period where plural systems - especially those in areas without access to treatment - are, indeed, functioning for years and years as multiples (or “Plural”). Even if you are able to find a good therapist, and begin treatment, therapy takes years and years. It makes sense that Functional Multiplicity would be a fantastic goal during this time, regardless of what the “end of treatment” looks like, we think. This is a quality of life issue, in those years after the trauma that caused the multiplicity (or “plurality”), the decades of waiting for help and access to treatment, and the years and years of treatment itself.
In regards to whether DID requires a trauma history, Dr. Barach went on to say that:
She said that there are people who have DID without a trauma history. Well, maybe so, but that is actually an empirical question--and where's the data? There are a number of published case series showing an extremely high rate of childhood trauma (like 95% or more) reported by people in clinical settings who have DID. There are also some people who believe they have DID, but actually they don't--they have just assigned names to aspects of themselves.
We would add that there may be Plural systems who deny trauma as part of the dissociative process, who just do not know yet about their own trauma.
That said, there are people who identify as “Plural” who report no trauma history, who say they have no disorder because they are not distressed by it and functioning just fine.
This is an important cultural development clinicians need to know about, whether they agree with it or not, just for cultural competency, that there are people in the “Plural Community” who do not consider themselves to have DID.
That said, if these people are functioning just fine and not distressed about being Plural, then they would not be seeking treatment for DID - which is likely why clinicians are less familiar with this (more recent) cultural population.
Finally, Dr. Barach responded to one last point:
Although the proponents of the structural theory may say that treatment should take place through the ANP, that treatment idea does NOT necessarily follow from the theory. And while the structural dissociation folks may be teaching therapists to work directly only with an ANP, that is not what a lot of other experienced teachers in the dissociation field are teaching (including me). I well remember Richard Kluft saying very clearly that you cannot treat someone with DID unless you are working with the "alters" (to use his preferred term).
In fact, when I reached out to Kathy Steele herself, to clarify what she was teaching from the slide used in the Stronghold System’s article, she was very responsive.
I try to work with the "adult self" to the degree possible, but do work with parts. I have a sequence of decisions on when you can work through the adult, when to work with a group of parts together and when to work with a single one, and then I work my way back up the ladder. I have never said I only work with the adult part or only ANPs.
We can say that we saw Kathy Steele present in Kansas City, in which the same slide used in the Stronghold System article was also displayed. But throughout the presentation, she did give many examples of how to work with different kinds of parts. So we followed up on this, and not only did she clarify further, but she also was eager to adapt her language so that would be more clear in the future what she meant::
I do emphasize that an "adult" needs to be active in therapy, which is maybe where the confusion comes in. By this, I do not mean any one part, but rather am focused on capacities necessary for successful therapy: the ability to contain behaviors, the ability to reflect, the ability to cooperate on mutually shared therapeutic goals. And in early therapy I always focus on helping the client as a whole to find those capacities and use them. I don't think any diagnosis - no matter which one - precludes these, and these capacities are either explicit or implicit in every single therapeutic approach.
I will think about maybe not using the term "adult" for these capacities to avoid further confusion.
This is why we do the podcast, for this kind of exploring and these kinds of conversations.
Working to understand the article on Power to the Plurals is important for understanding the client experience and cultural implications, while advocating for improved care and quality of treatment.
Working to understand the clinical response helps us to engage in treatment as we understand what is going on and why we are doing the things we are doing, and to better educate other clinicians and those still waiting for access to treatment.
This is empowering to us all, and a beautiful thing when we work together, even good practice at attunement and being receptive and attending to one another. Well done, everyone!